Hope Virgo fought for her life; campaigns for eating disorder support
Eating disorders present in all different shapes and sizes. Just because you can’t see that someone is visibly struggling, it doesn’t mean they aren’t.
- 5 years ago
July 31, 2021

LONDON, England — I developed anorexia when I was about 12 or 13-years-old. For me, it was something that had been brewing for quite a long time.
I grew up in a family where we had a lot of dysfunctional behaviors. I was also sexually abused as a child.
It started very slowly, restricting [food] here and there; and I upped all of my [long distance] running. The more I did [these unhealthy behaviors], the better I felt about things going on around me, and it numbed a lot of those emotions I didn’t want to feel.
In the evenings, lying in bed, I would listen to all the arguments going on downstairs. In those moments, I felt so low and so lonely; so stuck in my emotions.
My mind would always wander to the abuse and not feeling good enough. Because of the abuse and how I was treated, I felt there was something categorically wrong with me: no one stopped it from happening.
The eating disorder filled the gap and helped me feel like if I changed myself, something would shift. I was so taken over by the shame around [the abuse] that I started to detest myself; the eating disorder provided comfort in those moments.
I would have thoughts in my head that I’m not good enough or I’m not right the way I am. As soon as I felt any of those emotions, [my eating disorder] would immediately tell me to start thinking about food and calories and exercise.
I thrived off that and longed to do more of it. By that point, I had convinced myself that the more I listened to it, the better I would feel.
Reg flags lead to intervention
I didn’t think there was anything the matter with me at all. The school contacted my mom about my weight change.
I remember being in my doctor’s office thinking this is ridiculous; I don’t get why I’m here. Eventually, I was referred to Child and Adolescent Mental Health Services.
I sat through that first appointment not wanting to say anything or disclose what was going on. The guy was trying to get stuff out of me. I put up this complete and utter wall.
I left the appointment and went home and researched eating disorders and anorexia. I was convinced I didn’t have anorexia because I had this image in my head of what someone with an eating disorder should be like and how they should behave. I thought they didn’t like food. I thought they never ate.
I am based in the United Kingdom and we have access to the National Health Service here. I was entered into NHS treatment to try and not only get me to accept that something was the matter but to start to get the support I needed.
Over the next six months, I was placed in outpatient treatment but nothing worked for me. I spent those six months still in denial. I was so convinced people were trying to take away this one thing in my life that made everything feel amazing.
After six months I was admitted to an inpatient hospital where I then spent the next year of my life in recovery learning a lot about food and exercise. The biggest thing for me was learning to talk about how I felt.
Discovering my distorted thinking
Although my body image and my feelings about my body didn’t cause my eating disorder, those thoughts and feelings got so wrapped up in things. By the time I was admitted to treatment my body image was distorted.
I remember sitting in the hospital on this Friday night, so fed up and unhappy about being there. I did this exercise with one of the nurses. I had to draw an outline of my body – a life-size version of myself. Then she drew this life-size tracing of my body from me lying on the same piece of paper.
It was then I realized there was something wrong with my brain because the way I viewed myself was so distorted. I remember on that Friday night, I was like, I’m just going to start eating a little bit. Then I can at least get out of the hospital and do exactly what I want to do.
The next year, I began to talk about, process, and understand things. A starting point was having that space to talk; realizing that I didn’t have to show people that I wasn’t okay through the food; that it was okay to feel things.
So often when you have an eating disorder, you forget that it is a coping mechanism for life; that it is serving a purpose in the short time. The more I started to unpack that and think about it, the more I was able to shift a lot of that thinking and get to a place where I was able to process in more of a healthy way.
If I wanted to have the life I wanted to have, I would need to reframe a lot of things. I used to make so many lists of reasons to get well, my motivations, and the positives of eating. It was like ammunition that things were going to be okay if I kept doing what I was doing.
Unhealthy behaviors return
For over half my life I have had an eating disorder. I developed it when I was 12 or 13. I am now 31. I have been in a state of recovery since I was 17.
I have had moments when I thought maybe I was fully recovered, then I relapsed in 2016 following the death of my grandmother. I had a bad visit with her in the care home before she passed away and found the whole thing quite traumatic.
I felt like I let her down and let my mom down because I hadn’t been around for her to offer that additional support. When she passed away, I was so determined to be strong for everyone else that I pretended I was fine all the time.
I could feel myself going back into those unhealthy behaviors but was loving the short-term validation it gave me. I kept convincing myself if I did what I was doing, at some point I could completely switch it off and I could go back to full-on recovery mode.
That’s not how eating disorders work. You can’t get up one day and have an eating disorder and the next day decide you don’t want it to be there anymore. What I was doing was dangerous, getting back into that mindset again.
After a couple of months of struggling, I went to the eating disorder services in South London where I lived and tried to get support but unfortunately, because I wasn’t underweight, there was nothing they could offer me. That was when things began to go downhill quickly.
The road from relapse back to recovery
I would get up in the mornings and feel so unhappy, so emotionally and physically exhausted, and so stuck in what I was doing. I would go to work and put on a face, pretending I was fine. I would get home in the evening and cry a lot, just really struggling with life.

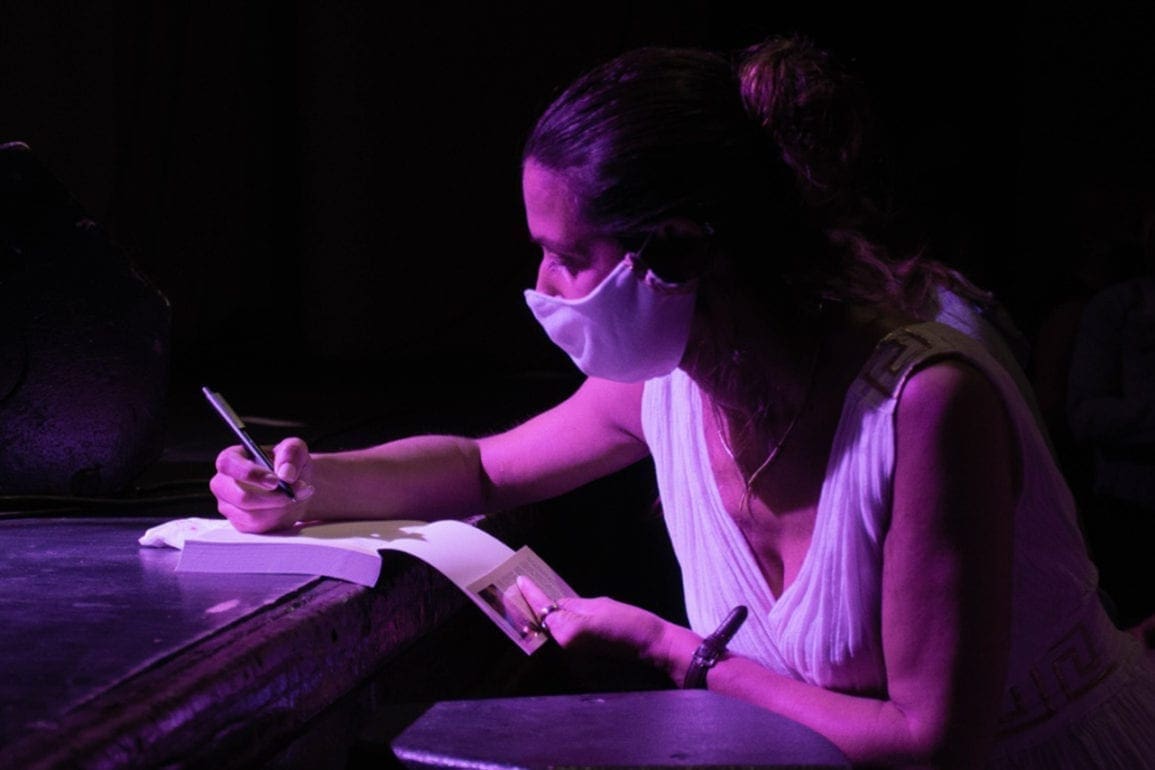
Prime Minister of the United Kingdom, where she went to advocate for her #dumpthescales campaign. | Hope Virgo
I went back to my doctor and they put me on anti-depressants to lift my mood a little bit. They definitely helped. I went on medication for about four years but also went back to that structure around my eating and my routine. I sat with those uncomfortable feelings I didn’t want to feel.
Eating disorders are such competitive illnesses. You don’t feel validated in your illness. For me, that’s what hits a nerve a lot of the time. This voice in my head was telling me you’re not sick enough; you don’t deserve this support. It was difficult to work out what to do and how to manage.
I have made a lot of mistakes in my recovery. I do not know what the long-term effects of my eating disorder will be on my body, but I am now doing everything I can to shift things; to get to that space where I will be fully recovered.
I started journaling a lot; writing down all my feelings and emotions. Having that space, particularly in the evenings, to offload helped. I booked loads of nice things to do with my friends as a distraction, to create happy memories, and get out of my head.
Something that always helped in recovery was being able to travel. It is a massive motivator for me. I also learned to talk about things.
To others struggling
Over the last year and a half, I have stepped up my recovery and I’m pushing for this final phase. I work with a dietician. With her, it’s unpacking food beliefs and making sure the behaviors support the outcomes I want with my life.
Just after Christmas, I decided something I want to be able to do when I have children, is go for a last-minute pastry with the kids. Every Friday morning since Christmas, I’ve gone out for a pastry. At first, it was really difficult and I got upset about it. The more I did it, the easier it got and I gradually began to trust myself and shift the thinking in my head.
[To others struggling], I would first ask what the eating disorder behavior is doing for you. Take a little bit of a step back and ask yourself, “Do I want to spend the rest of my life feeling like I have to do this?”
Your feelings matter. Yes, life can be difficult at moments. What the eating disorder is doing for you and how it is making you feel is a short-term solution.
Try and think about what you can put into place whether that is going to therapy, talking to your doctor, telling a friend, or booking fun things to do. Start challenging the thinking.
So often with eating disorders, we get stuck. We label foods as good and bad. We are afraid of pushing things out. If you are in that situation now, stop for a moment and think. Yes, it feels like I’m scared of it. Yes, I’m worried about what this will do to my body.
That fear is so unfounded. If I work through that fear and those feelings around food, I’ll get to have the life I want and deserve. Don’t wait until you are at that so-called crisis point.
Advocacy work: a new purpose
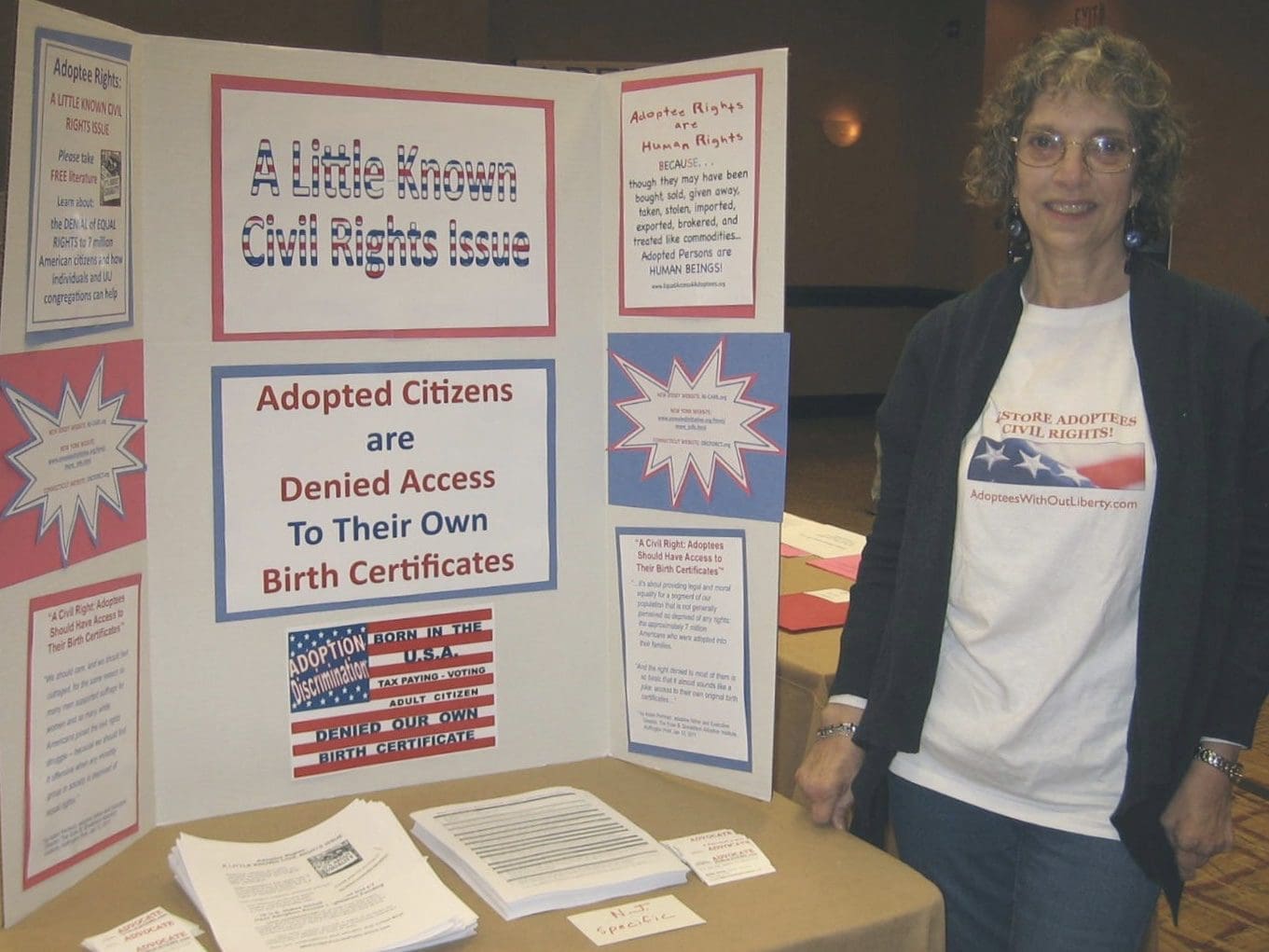
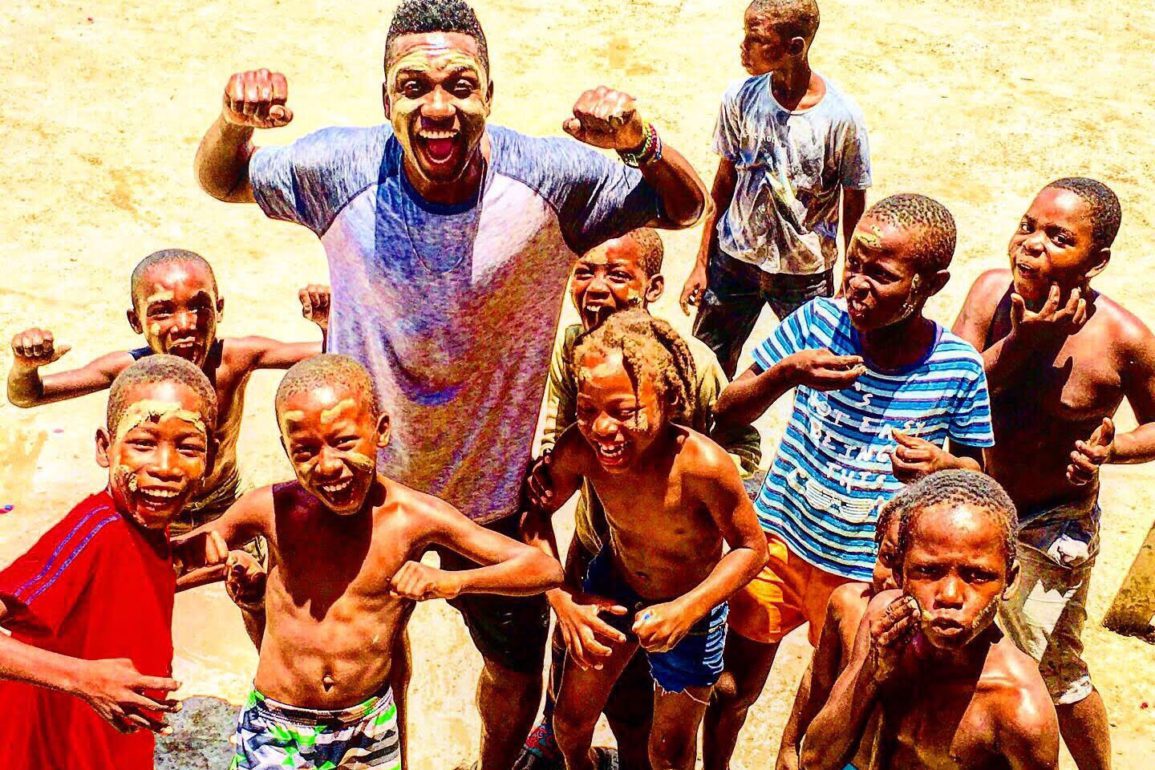
Today, I work full-time doing mental health campaigning. I spend my life traveling all over the world, working with schools, corporations, hospitals, and the government in the UK.

I look predominately at issues around eating disorders and diagnosis but also more broadly at that whole spectrum of eating disorders, disordered eating, and mental health.
A huge part of my work is trying to get people to understand that eating disorders present in all different shapes and sizes. Just because you can’t see that someone is visibly struggling, it doesn’t mean they aren’t. I am trying to shine quite a big light on that so every single person, regardless of what they look like, can get the support they need.
I am in an ongoing state of recovery. I do believe every single person with an eating disorder can make a full recovery if they get the right support and the right interventions. I am still on the journey of hitting that marker.
Most recently I set up a steering group called the Hearts, Minds, and Genes Coalition where we are looking at bringing together the genetics, the nature side, the nurture side, and the heart, to try and marry up that eating disorders are a mental illness but present with physical outcomes.
I also have a campaign called Double the Scales to make sure people can access support and treatment regardless of their weight or body mass index. It is a UK petition but [this issue] affects people all over the world.
How to support someone with an eating disorder
I often reflect on the fact that I spent that year in the hospital and was extremely privileged that I got to have a space in treatment. Worldwide, we are seeing this massive influx of people struggling with eating disorders. The lack of care and support is just awful.
Remember, you do not need to fix that person. We don’t want to be fixed. We don’t want sympathy. We just want someone to walk alongside us and offer space to talk things through, if we need that distraction around mealtimes, or are feeling anxious. We want to feel heard and really understood.
I believe in direct conversations. We shy away from them because they are difficult or might upset someone. The more we bring these behaviors out into the open, the more people are likely to get that full freedom and start to recover.
So, have the direct conversation, offer support, distract them, be patient, don’t judge, and don’t just see the eating disorder when you look at them. Often it becomes someone’s whole identity which is just not right.
There is so much more to that person than just an eating disorder. Whether they are struggling, in recovery, or living with it and not realizing it, there is another side to them. We need to work to help them see that and love life again.