Israeli paramedic sees trauma, riots, heart attacks on either side of ceasefire
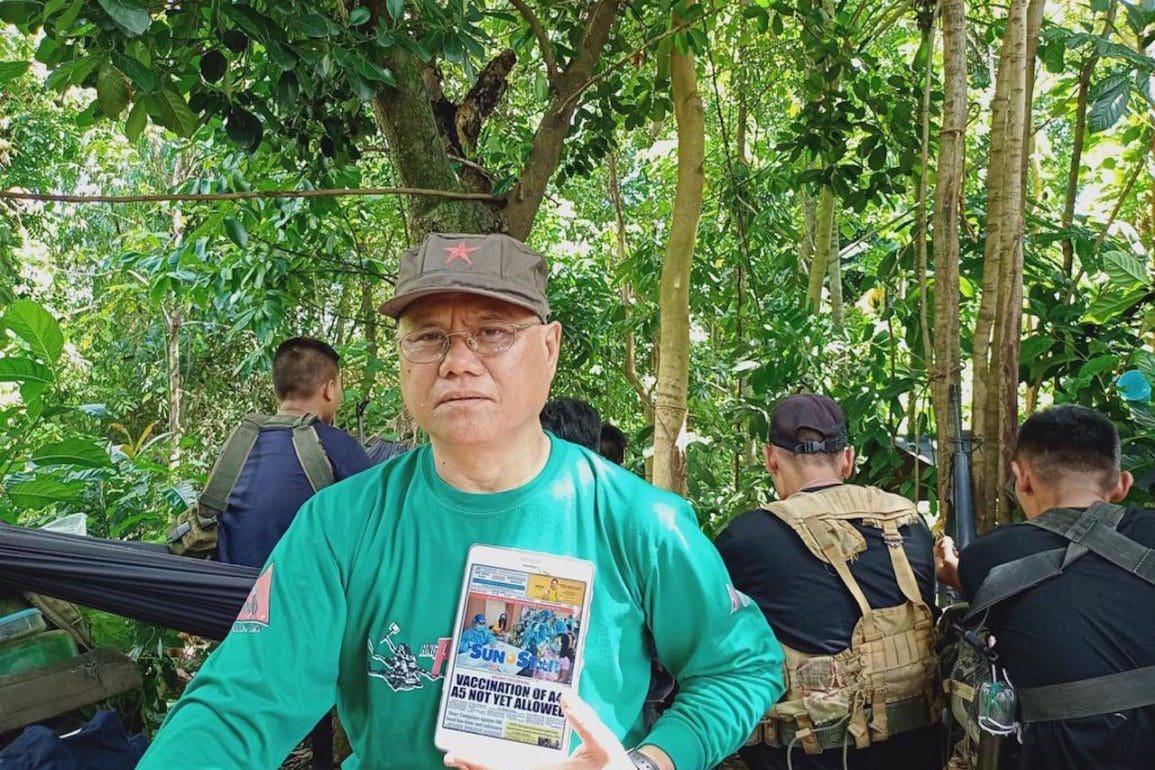
While I was resuscitating a patient, an air raid siren went off alerting us to incoming rockets.
- 5 years ago
June 8, 2021

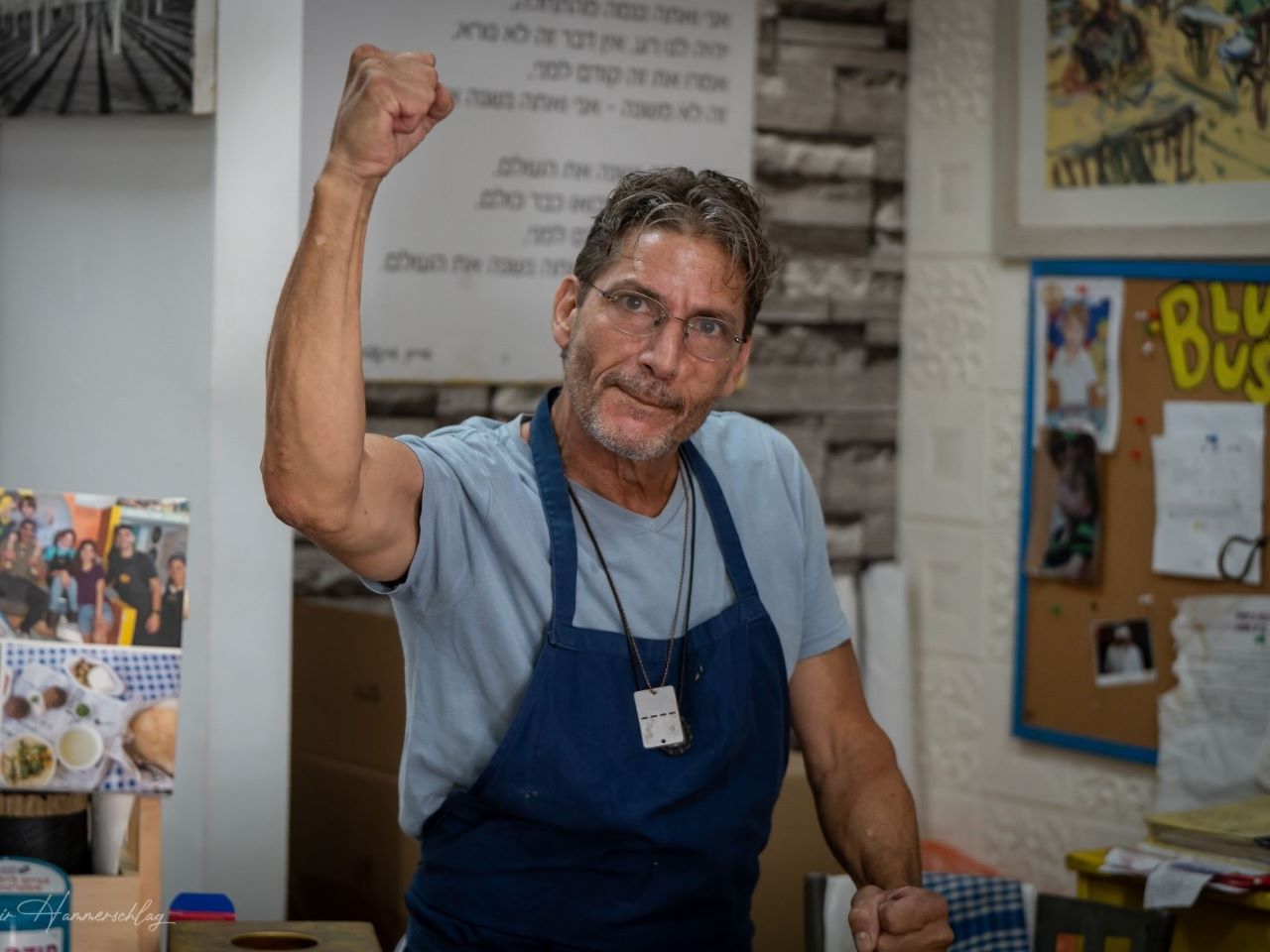
LOD, Israel — Paramedics in Israel respond to two distinct types of emergencies: routine emergencies, like heart attacks, and extreme emergencies, like rocket fire and riots.
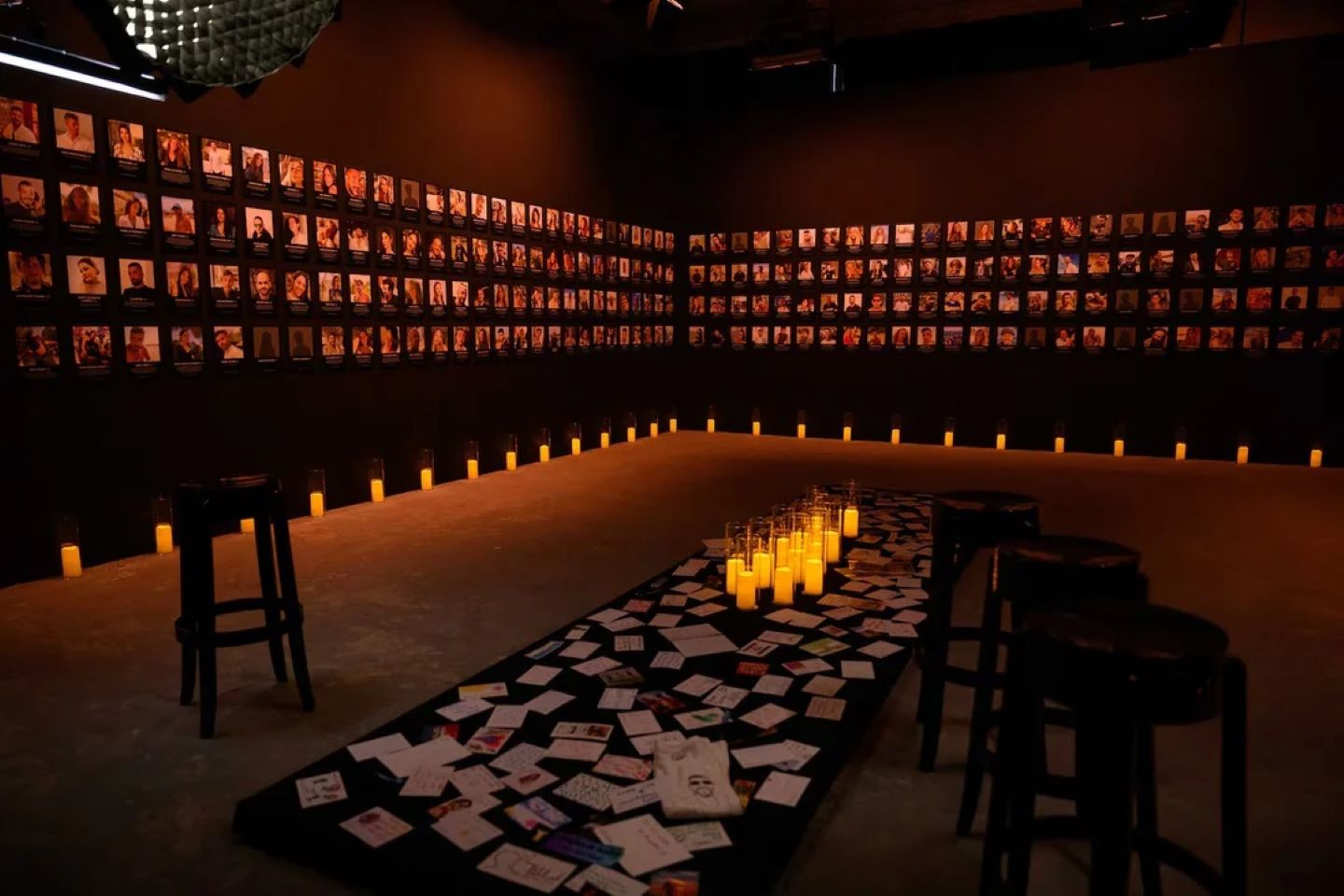
In the seven days following the May 20th ceasefire between Israel and Hamas, I responded to a string of suicides.
Though categorized as routine, we were unable to save the patients in any of the suicide attempts we responded to.
Instead, we take on the role of comforting the family of the deceased.
We’re all human and we’re treating human conditions. I see things a normal person may not see once in their lifetime.
Raw emotions
When responding to a routine emergency, I encounter incredibly raw emotions.
Even if you’re the best trained and most skilled paramedic, being in those moments places an enormous weight on your heart.
On one hand, I’m standing there as an outsider. On the other hand, I’ve just given this patient’s family the worst possible news while assisting them in their home.
I try to find a way to leave the family feeling that if there was anything we as paramedics could have done, we would have done it.
Sometimes I take that away with me.
If I were to make a guess as to why there have been multiple suicides, I would say the declining national mood following security incidents in Israel has pushed some people over the edge.
While it could be a coincidence, this is my best guess.
Worst day of their life
The toughest part of being a paramedic is arriving on the worst day of a person’s life and giving a family the worst news they could possibly hear. I meet with them during these intimate moments.
Very often, I don’t know the outcome of our patients after we drop them off at the hospital.
I think any paramedic who says they’re not affected by the sights, sounds, and smells of what we’re exposed to is potentially lying to themselves.
Thankfully, I have learned not to be affected during the actual on-the-job response. When I’m on the scene, in the midst of a crisis, my first-responder training kicks in.
Later, I take home the trauma with me. It is then, as a paramedic, I have to respond to my own emotional crisis, like I would an emergency call.
We cope by talking with someone, going running, playing music, or writing, for example.
Whatever the coping method, it is very important to make a differentiation between work life and home life.
Get into mindset
When I respond to a routine emergency, I quickly get into the mindset of what I’m about to face.
Am I facing somebody who is having difficulty breathing or having a heart attack? Will we be delivering a baby?
No matter the call, I have to get myself into the mindset of the emergency.
I focus on getting to the scene of the call, trying to save lives, and stabilizing patients.
When I’m responding to an emergency call during periods of conflict, there’s an added level of caution.
I could be facing someone who has been injured by gunfire or rocket fire.
While we’re trained for these events, rocket attacks are certainly unfamiliar territory for us.
Personal risks
As a paramedic, I take personal risks and there is an element of fear.
I am equipped with helmets and protective vests.
I have to prioritize my own life and the members of my team while we are trying to save people’s lives.
On May 13, in Modi’in-Maccabim-Re’ut, adjacent to the West Bank, I was responding to a routine emergency call for cardiac arrest.
The patient’s heart wasn’t working.
While I was resuscitating the patient, an air raid siren went off alerting us to incoming rockets.
The team of paramedics and I took cover as we moved the patient to a safe room.
Safe rooms
For the past 20 or 30 years, every home or apartment in Israel comes equipped with a safe room made with heavy steel doors and metal window shutters.
We continued the patient’s resuscitation while waiting for the siren to go off.
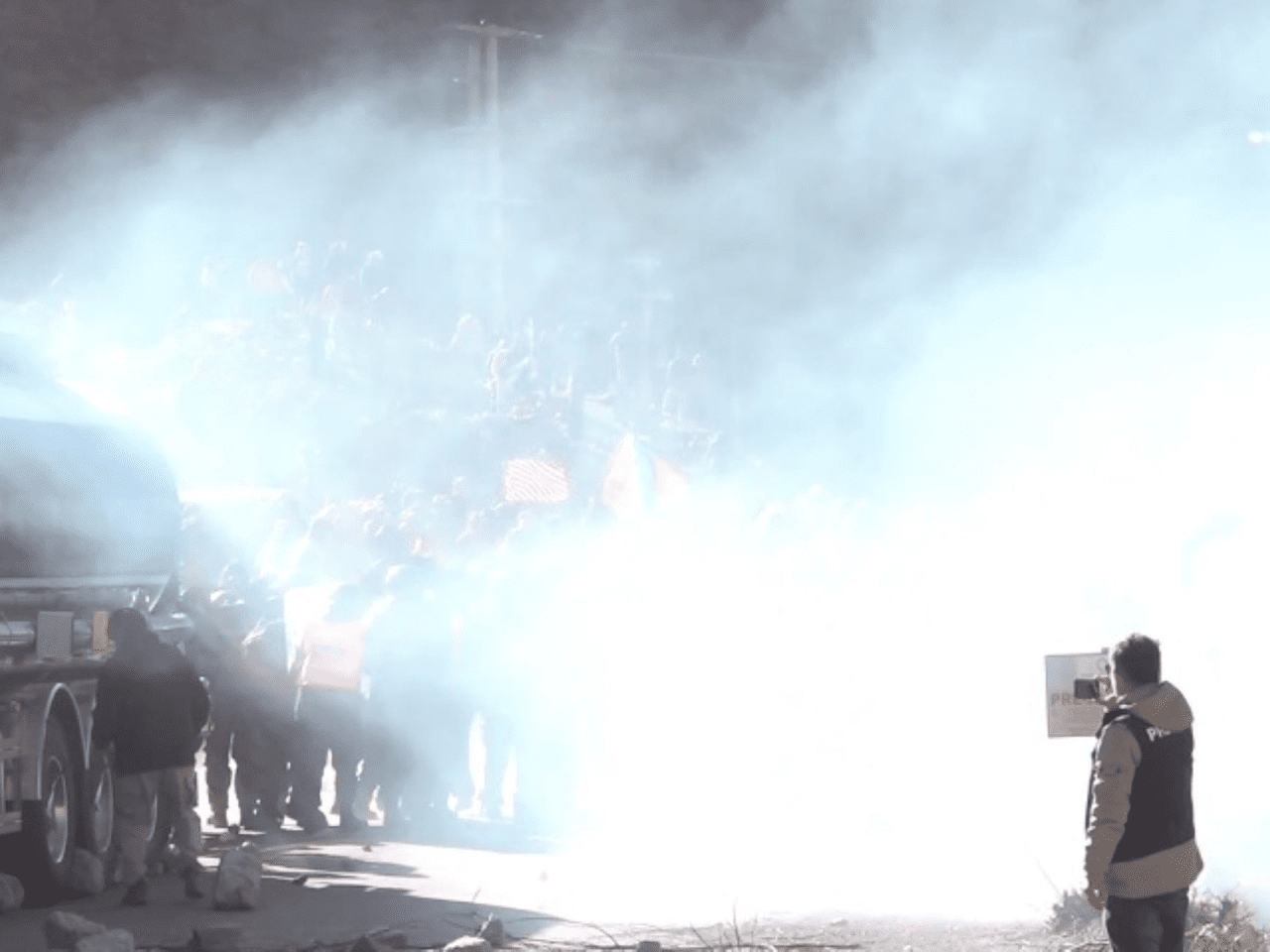
Unlike the air raid sirens alone, unrest within Israel is also responsible for extreme emergencies.
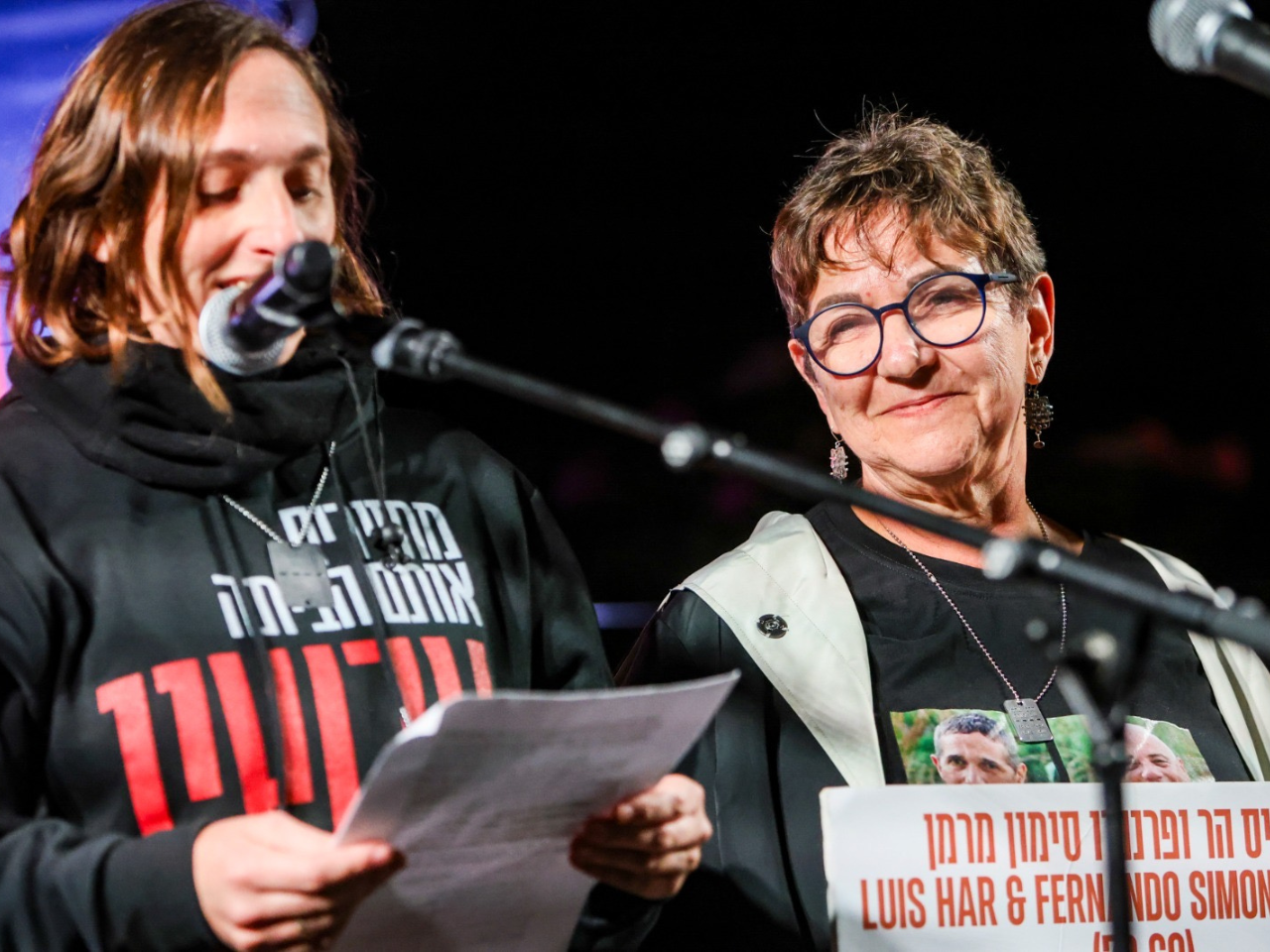
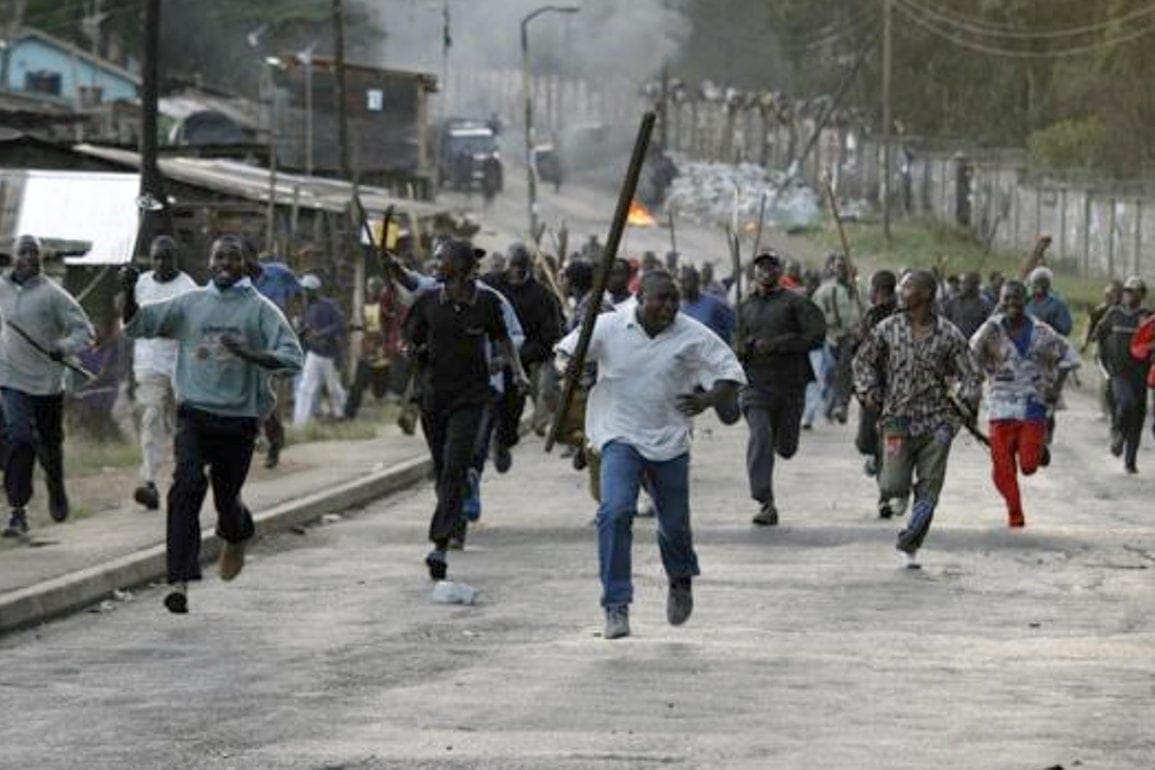
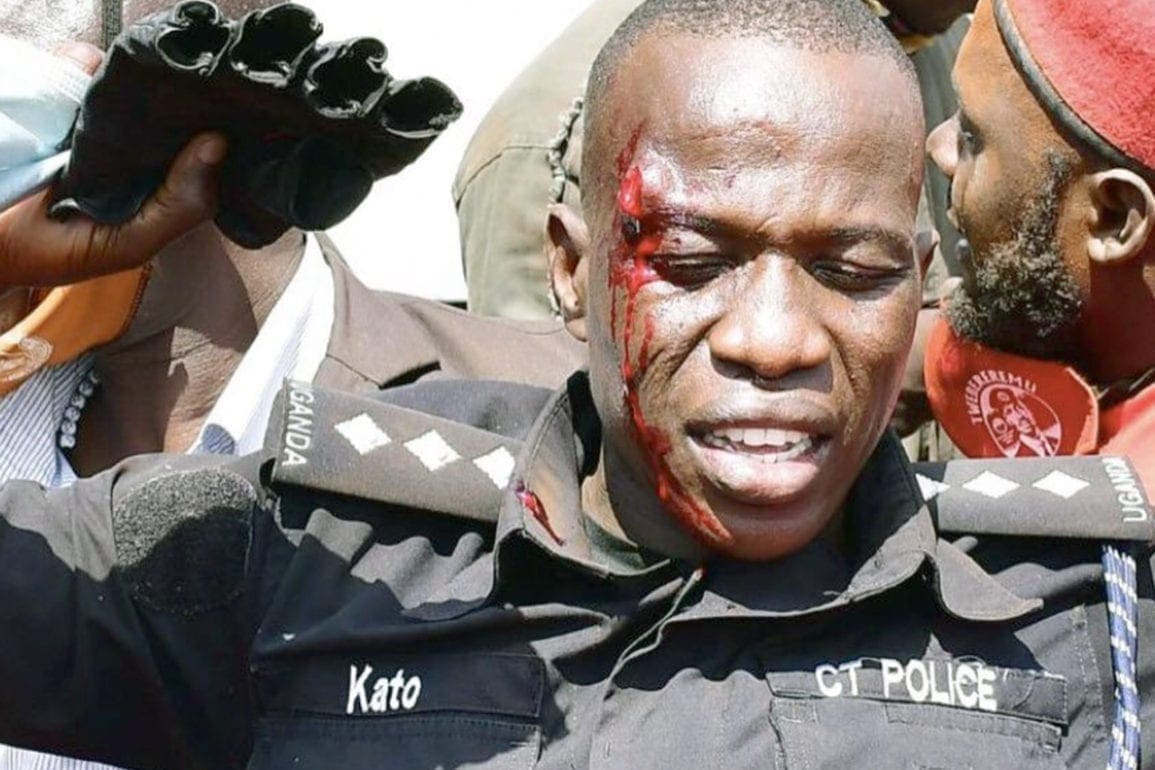
Riots between Israeli police, Israeli Arabs, and Israeli Jews broke out on May 12 in Lod, prompting the government to declare a state of emergency.
I was called to the scene that day and treated several patients who were injured in this civil unrest, some severely injured.
There were protesters who were also killed.
A way to give back
I became a paramedic because I wanted to have influence on the world around me, a life-saving experience, and a way to give back to the community.
On one hand, being a paramedic is a daunting prospect, on the other, it’s a great privilege.
People invite me into their homes without knowing who I am. They trust me with their lives.
Working for Magen David Adom is a humbling experience.
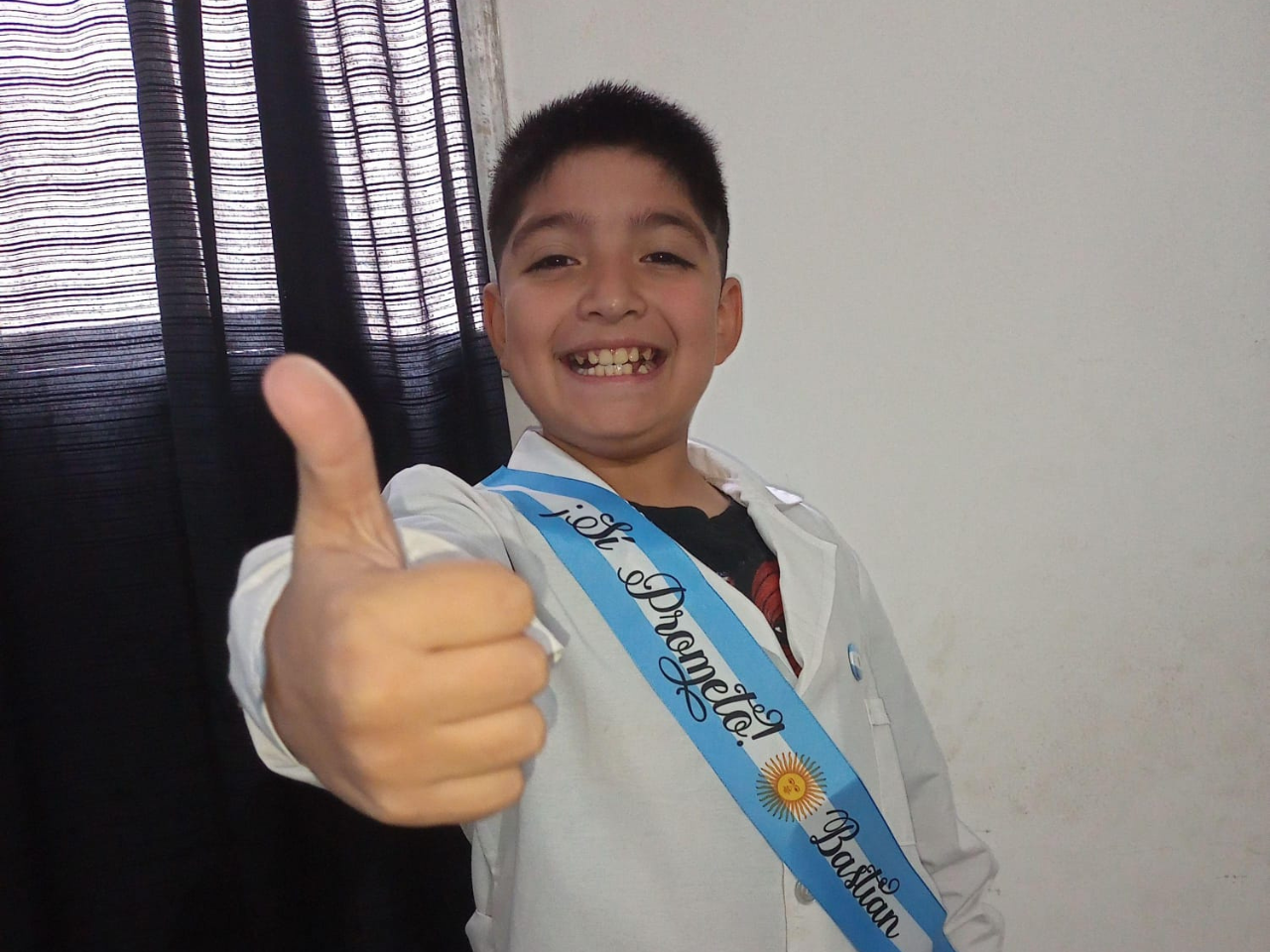
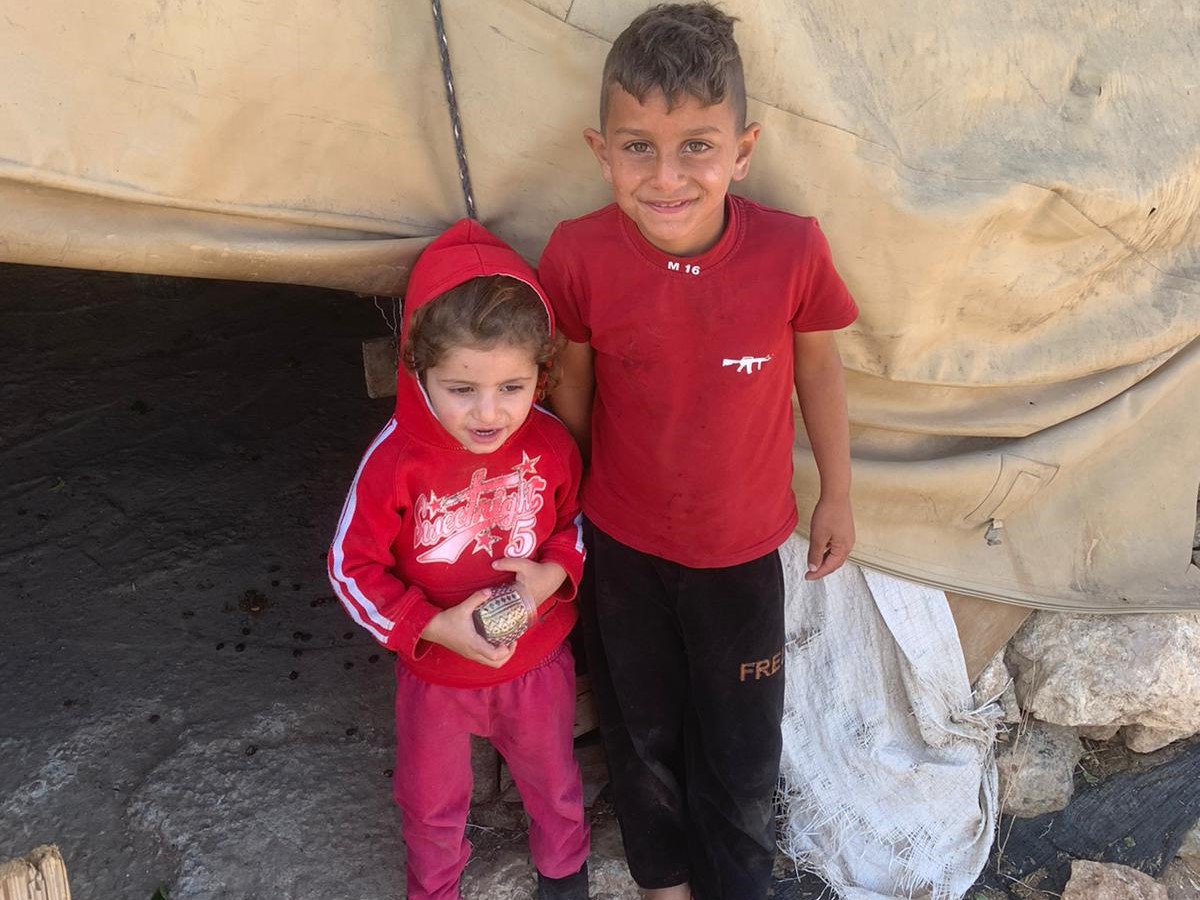
Israeli Jews, Israeli Arab Muslims, and Israeli Arab Christians make up Israel’s national paramedic service, Magen David Adom, much like the country’s civilian population.
The service has approximately 2,000 employees and tens of thousands of volunteers.
The volunteers range in age from people in their 20s and 30s well into old age, including one 90-year-old.
Magen David Adom relies on donations from mostly outside of Israel and Israeli benefactors, on top of user fees from the patients.
The financing keeps us responding to all kinds of emergencies, routine and otherwise.